Answers Your Questions on Hemianopsia
Click here to learn more about Dr. Windsor
Will my hemianopsia go away in time?
During the first three to six months, there is a possibility of some improvement, but this occurs only in a limited number of patients. In careful studies on two separate groups of patients totaling over 300 patients, Zihl found small amounts of recovery of the visual field in only 12% and 16%. Only 4 patients in the second study of 225 patients over three months showed complete recovery. Thus small improvements may occur, but in only a small number of patients.
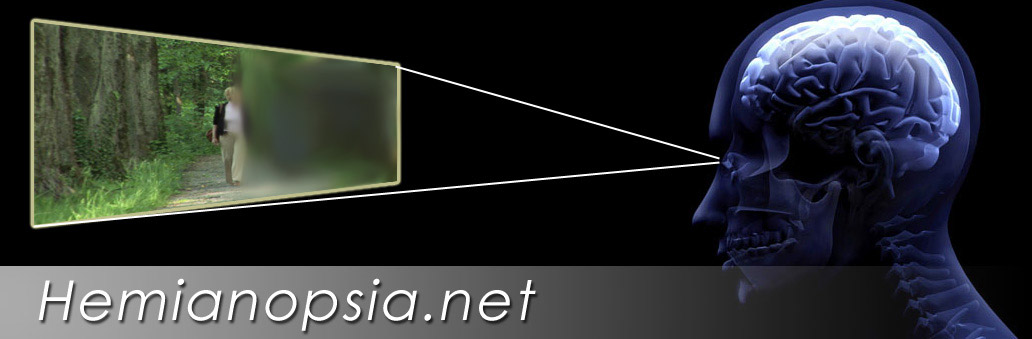
Does a patient with a hemianopsia see "black" where the field is lost?
No. This is a misconception unfortunately still presented by people who attempt to demonstrate what a hemianopsia is by blacking out the area. Notice the head graphic on this page. Notice that the lost area seems to blend with the scene. The loss from hemianopsia is just a void in the vision. The patient does not see it as black, but rather the brain fills it in perceptually to blend with whatever the patient is viewing. We all have a small blindspot about 15 degrees to each side in each eye. We do not see these as black spots. They appear to blend with what we are looking at. Another example is that our eyes look straight ahead. We do not see behind us, but we do not perceive this as black but just a void in our perception.
How soon do you recommend treatment on a new hemianopsia patient?
As soon as the patient is stable and adequately recovered, in-hospital occupational therapy including saccadic eye movement training may be initiated for visual field loss and therapy for visual neglect if present. Because in the first few months there can be some mild improvement among some patients, the use of visual field expanders may be delayed slightly until we are sure that the condition is stable.
It has been our experience that in a complete dense homonymous hemianopsia remaining after four to six weeks, the possibility of spontaneous improvement is very low and visual field expanders can be considered. Each case, however, should be looked at individually.
Why am I startled so easily when people approach me from the side of my hemianopsia?
As we walk down a sidewalk, our peripheral vision detects things occurring around us in an almost unconscious way. A bicyclist approaching from the far left would be detected long before it crosses our path. However, if you have a left homonymous hemianopsia, the bicycle will not be seen until it suddenly emerges from the blind side straight in front of the patient. Constantly being startled can lead the patient to become uneasy in travel.
Is it normal for my vision after a hemianopsia to seem hazy or foggy?
Our contrast sensitivity function allows us to see subtle boundaries like a grey pen on a dark grey desk. This ability is often impaired after a brain injury. The patient may experience it as haziness to vision and it may make them more sensitive to the interference of glare.
Is it normal to be very sensitive to light and glare?
Both our ability to handle low light and high light levels may be affected in homonymous hemianopsia patients. Some patients may require higher contrast filters in their general eyewear as well as sun filters outside. Blue-blocker type filters should be considered.
Why do I see sparks and flashes in my vision?
After suffering an acquired brain injury including stroke, trauma and brain tumor some patients will see sparks and flashes and other unformed visual hallucinations. These are most commonly immediately after the event and may lessen with time. Patient may also see formed hallucinations.
.
Why is my night vision so poor after my stroke and hemianopsia?
Our adaptation to light and dark can be impaired in hemianopsia patients. The hemianoptic patient is also losing half of his or her peripheral vision which has a predominance of rod cells that help us see at night. Additionally some medications, such as some given for seizure disorders, may effect night vision.
Is it normal to be fearful to travel? I feel like I just want to stay in my home.
Many patients struggling to overcome problems with hemianopsia such as running into things, being startled, and feeling disoriented in crowded areas. Patient become fearful not only of injuring themselves but of looking impaired in public. They often gradually restrict themselves more and more to their home.
Why do I have trouble finding things on my desk in a cabinet or in the refrigerator?
The hemianopsia to one side or another is essentially blocking half of your view. When we open a cabinet fr example, our peripheral vision picks up what we are trying to see and you make one large sacaddic eye movement to find it. With this type of visual of loss, you may have to scan and search much harder to find it since your peripheral vision can no longer help you.
Since his stroke my father runs into things and trip and fall, but he continually denies to me, and his doctor that he has a problem with his visual field. Why does he deny his visual field loss?
Some patients who have a brain injury may not realize what they are not seeing. This is the inability recognize that they have had a stroke or a brain injury and the problems that are associated with it. This is quite common in patients with right sided damage, left homonymous hemianopsias and visual neglect.
What is the difference between a left homonymous hemianopsia and left visual neglect?
A homonymous hemianopsia is a true loss of the sense of vision from damage to fibers that carry the signals to the visual cortex or damage to the visual cortex.
Visual neglect is a loss of attention to one side of the body, almost always the left side of the body. It can extend beyond vision and include memory of objects normally to that side. It is crucial that the visual field testing be combined with tests of visual neglect to arrive at a proper diagnosis before treatment.
Can you have both visual neglect and a hemianopsia?
Yes! Both visual neglect and homonymous hemianopsia frequently do occur together, but a patient can also have either alone. It all depends on the exact location of the damage in the brain.
What are the signs of visual neglect?
Signs may include a disregard for the patient’s left side. The patient fails to direct attention to the left. The patient may orient himself or herself more to the right side. Many functional skills will be disrupted including reading.
Why can my father not recognize faces since his stroke?
This may be a relatively rare condition called Prosopagnosia. It related to damage to the Fusiform gyrus in the Temporal lobe of the brain. This area is needed to recognize familiar faces and to remember new faces. The patient may need to rely on other senses, primarily hearing a familiar voice to recognize a person. Announcing your presence will help.
Why, since my right hemianopsia occurred, I can read individual words, but struggle to read down a line of text?
In the case of a right homonymous hemianopsia that splits directly through the macular region, parts of large words to the right side may be lost. Since in English, we read from the left to the right, we automatically start by fixating at the start of words. This causes the ends of large words on the right side to disappear as well as the end of the line of text. In this website, we discuss several ways to resolve this problem.
Why do I loose my place in reading a line of text?
A hemianopsia typically runs directly through or very near the center of our vision. If the patient has a right field loss, then as the patient reads down the line, the end of the line is hidden in the blind area. The patient may frequently think the end of the line has been reached and return to the next line only to find that what they read did not make sense.
If the patient has a left visual field loss, they can see to reach the end of the line, but the blind spot to the left side blocks their view of the start of the next line. When the patient starts to return to the next line, they may stop too soon and miss the very beginning of the line. Thus visual field loss often results in the patient feeling very frustrated and may lead them to discontinue reading. On this website, we show the methods of aiding these reading problems.
Why do I no longer have a good sense of direction?
If the parietal region of our brain is affected, usually on the right side, our ability to understand and interpret our visual environment may become impaired. Add to this the loss of visual field on one side and the patient may feel very disoriented and may feel confused navigating a path.
Is it normal for my eyes to seem dry or feel gritty or sandy?
Dry eyes, due to slowing of the blink rate after brain injury, are very common after an acquired brain injury. The use of artificial tears may be beneficial as well as new prescription drugs such as Restasis and Fresh Kote may be used to improve comfort.
I am 25 years old and suffered a brain injury in an automobile accident. Why can I not seem to focus to read clearly?
It is crucial to our reading that our eyes either focus on the text to make it clear or that lenses are used to bring it in to focus. Loss of our focusing ability usually happens naturally in our forties, but it is not uncommon in young patients after an acquired brain injury. Younger patients, those under age 40, may notice difficulties in accommodation, the ability to focus the eyes. A simple bifocal can resolve this problem.
Why since my brain injury from an automobile accident do I have double vision?
In trauma to the brain, it is not uncommon that the nerves that control the eye movements or the control center in the brain may be damaged. This may result in double vision since both eyes cannot be controlled to work together. Prisms to move the images together, orthoptic therapy or eye muscle surgery may be indicated. Patching may be required in some cases, however black “pirate” patches should never be used. Newer patch methods on the eyeglasses including the Mins lens are advised.
Can a visual field expander prevent me from being startled so much?
Visual Field Expanders can shift the image from your area of vision loss to your sighted area. Patients report that they are startled less often with objects suddenly appearing out of their blind side with a field expander. They notice them as they approach with their field expander.
Will visual field expanding eyewear cure my hemianopsia?
No! It does not cure your loss of peripheral vision, but it does improve the patient’s functioning. For many patients but not all, visual field expanders can improve their day-to-day functioning, too let them travel with more safely, lesson bumping into things, and makes them less apprehensive in crowded areas. In a small number of cases, it may let them return to higher functions, such as returning to work or to drive again.
I had my stroke 5 years ago, but I am still struggling with bumping into thing, being disoriented and easily startled. Can I be helped with a visual field expander?
While some patients adapt quickly to their hemianopsia, other continue to struggle for years. Even after saccadic eye movement therapy, they still struggle. We find that these patients are often ideal candidates for the newer forms of visual field expanders such as the Gottlieb VFAS, EP Horizontal, or Chadwick Hemianopsia systems.
Do all people with homonymous hemianopsias benefit from visual field expanders?
No. While we can help many patients with visual field expanders, some patients adapt to their visual field loss quickly and function well without them. It is also dependent on the patient’s goals. A retired individual staying at home and functioning well within this or her home may not benefit as much as a patient who wishes to return to work or drive.
I tried press-on prisms on my glasses years ago and i didn't like it. Are systems different now?
Unfortunately, press-on prisms have been over used and often in manners that were not effective. The modern visual field expanders have better quality of the image as they are made of high quality optical plastics. Additionally, in the past prisms were placed on both eyes. We know today that that is not an effective method. The new types of visual field expanders, when prescribed by doctors experienced in hemianopsia rehabilitation and combined with appropriate saccadic eye movement therapy provide better outcomes.
After my stroke, they put press-on prisms on half of both of my lenses. I understand that is no longer the recommended method.
Forty years ago, it was common to apply a press-on lens on both eyes. Since the 1980s with the introduction of the Gottlieb VFAS lens and later in studies done by Dr. Eli Peli, senior research scientist at Harvard’s Schepens Eye Research Institute, it has been clearly shown that only monocular visual field expanders create a true visual field expansion.
Today bilateral visual field expanders should not be used in the treatment of homonymous hemianopsia.
What is the difference between a press-on prism and true ophthalmic quality visual field expanders like the Gottlieb VFAS, EP Horizontal or Chadwick lenses?
Press-on prisms are helpful to demonstrate the concept of visual field expansion but are made of a soft plastic that lacks the clear bright quality of the ophthalmic materials used to make the newer visual field expanders. Many hemianopsia patients also have a loss of contrast sensitivity, thus adding a press-on lens further reduces the patient’s contrast sensitivity.
Many hemianopsia patients benefit significantly from brighter and higher contrast of the Gottlieb VFAS or Chadwick Hemianopsia Lens. One exception to this concept is the EP Horizontal lens. It has better contrast than a press-on lens, but somewhat reduced contrast compared to the carrier lens. Because the EP Horizontal lens is a simultaneous system, the slight reduction in contrast helps differential the carrier image from the visual field expander images.
What is a press-on visual field expander?
Press-on prisms are thin wafers of soft plastic that replace a thick prism with a series of very small thin prisms molded into the surface. The advantage is that they are inexpensive, but the disadvantage is the reduced contrast through the prisms. In our practice, we do not recommend press-on prisms for those with potential to drive, as hemianopsia patients often already have impaired contrast sensitivity and thus need maximum contrast through the lens. Press-on prisms are very helpful to place on existing eyewear to demonstrate the concept of visual field expansion.
What is the examination process for a patient with a homonymous hemianopsia?
The examination of a homonymous hemianopsia patient begins with an extensive medical and functional history. A full eye health examination is performed and low vision refraction is done to measure the prescription. Tests of visual fields, visual neglect, and visual spatial perception may be performed. A careful assessment of the eye movements and binocular vision is performed. Special testing is done with visual field awareness systems to determine if the patient can benefit with the system. Issues of glare and contrast sensitivity will be addressed including the use of high contrast filters.
The doctor will then develop a rehabilitation treatment plan and discuss this with the patient.
How do visual field expander help hemianopsia patients?
Visual field expanders work by shifting the image from the impaired side into the side with remaining vision. As the patient uses the visual field expander, he or she samples the information from the impaired side and creates an awareness of what is happening on that side. This can lessen running into things, being startled and can improve functioning in day-to-day activities.
What is Saccadic Eye Movement Therapy?
We use our side vision to maintain our awareness of the world about us. It allows us to safely move through our environment. In a homonymous hemianopsia, the patient has lost half of their visual field. One of the first ways to improve functioning with a hemianopsia is to teach the patient to scan into the area of the loss. This shifts the existing visual field to that side, helping the patient to detect objects within the area of loss. Areas that control these eye movements, called saccades, are often damaged at the same time the sensory loss occurs, making therapy even more important.
What is Vision Restoration Therapy?
Vision Restoration Therapy is a new treatment based on the concept of neuroplasticity of the brain. It is an exciting concept. However, it is still a controversial treatment owing to recent studies that show much less improvement than the original published studies. It involves using a computer-based system to stimulate of the boundary of the vision loss daily over many months.
How do you adapt the car to drive with a hemianopsia?
Additional mirrors may be added to the car. A panoramic mirror can fit over the existing rear view mirror. It can be angled slightly in the direction of the field loss. Another small mirror can be place to help pick up movement in the side window. Additional small panoramic mirrors can be added to the outside mirrors. It is important, however, not to add too much complexity to the driver’s environment. The driving rehabilitation specialist should evaluate the patient’s ability to use these additional mirrors safely.
Who provides drivers rehabilitation training of individuals with hemianopsia?
Certified driving rehabilitation specialist experienced in working with hemianopsia patients should perform the driver’s training of hemianopsia patients. The training of a patient with hemianopsia requires a special understanding of the issues these drivers must address.
What type of driving rehabilitation will I need?
It depends on the extent of your problems. The training can include, but is not limited to dealing with different types of crossings, pedestrian detection, lane positioning, changing lanes, maintaining appropriate gap, going on and off interstate highways, defensive driving techniques, and recognition of dangerous situations.
I have been told not to drive because of my visual field loss, but I passed the visual acuity test at the bureau of motor vehicles and I am driving. Will my insurance cover me if I have an accident?
For legal advise, you must consult with your lawyer. Even if you are licensed to drive, if you are aware of a new serious unaddressed problem that effects your driving negatively or have been advised to not return to driving by your doctor, you may not be fully covered by your insurance. In the case of an accident settlement, your insurance company could sue you for contributory negligence. We advise all patients with hemianopsia or other acquired brain injuries to not drive and only return to driving after appropriate therapy, driver's rehabilitation and being released by your doctor.
My husband has attempted to return to drive on his own without the doctor releasing him or driver’s training. Why do I notice that he tends to drive too close to the right side, but he argues that he is in the middle of the lane?
Patients with homonymous hemianopsia frequently misjudge the straight-ahead position with a consistent bias to one side. In driver’s training these tendencies are dealt with on the road. The patient must learn to understand his misperceptions and compensate by shifting slightly away from the bias direction. Curves can be a more difficult area for compensation.
If I I am fit with a visual field expander can I then drive again?
Driving is a complex process and requires consideration of many factors. We can help a small number of high functioning homonymous hemianopsia patients. But these individuals must be free from other problems that could also impact their driving ability. Areas that must be assessed include visual neglect, cognitive skills, physical stamina, processing speed, seizure status, medications, and status of hemi paresis. Additionally, the ability to scan into the area of loss and the ability to utilize the visual field expander must be determined. Then behind-the-wheel driver’s training with a certified driving rehabilitation specialist is required. Additionally, your state law must not restrict you from driving with a homonymous hemianopsia.
How can get more information or arrange an examination to determine if I can be helped?
To arrange an appointment with one of our doctors, please contact our Indianapolis office (317) 844-0919. They can assist those traveling from outside the state and International patients in finding lodging.
Please contact us if you have any questions.
The Low Vision Centers of Indiana
Richard L. Windsor, O.D., F.A.A.O., D.P.N.A.P.
Craig A. Ford, O.D., F.A.A.O.
Laura K. Windsor, O.D., F.A.A.O.
Ali E. Prible, O.D.
Indianapolis (317) 844-0919
Fort Wayne (260) 432-0575
Hartford City (765) 348-2020